CD Laboratory for Image and knowledge dRivEN prEcision Radiation Oncology (IRENE)
Head of research unit

Commercial Partner
Duration
Thematic Cluster
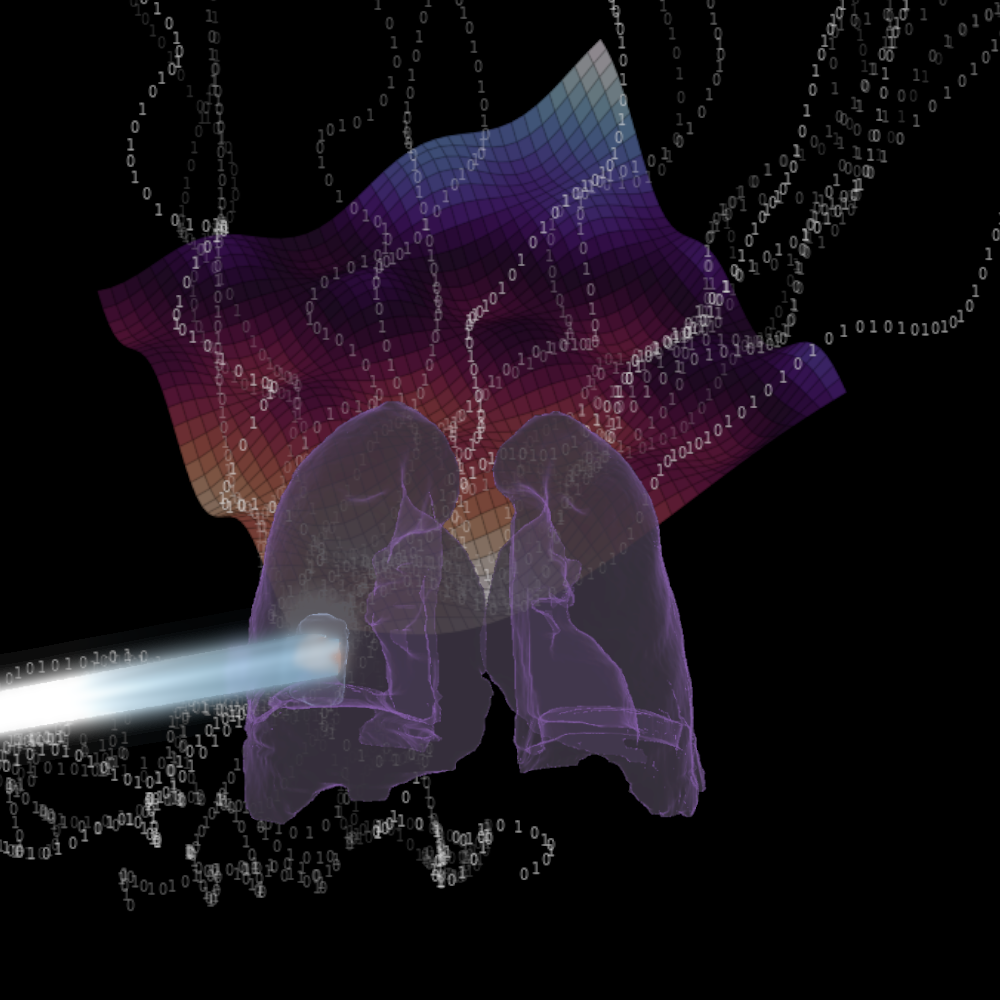
The aim of this CD Laboratory is to improve radio-oncological treatments, i.e. the irradiation of tumours by combining new technical approaches in (real-time) imaging, tumour-biologically oriented adaptive treatment concepts and automated prospective data acquisition in order to be able to offer all patients individualised therapy.
Despite significant advances in radiation oncology, which now make it possible to irradiate the area to be treated very precisely, most of the current standard treatments are based on a "target area definition" immediately before the start of treatment. Changes during or in the course of the therapy, which can sometimes last several weeks, are generally not taken into account or are compensated for by a larger radiotherapy volume. The CD Laboratory therefore focuses on increasing the precision of radiotherapy with regard to possible tumour movements during or changes in the tumour during the course of radiotherapy, tailored to each patient.
In the case of lung tumours, for example, tumour movements and anatomical changes can occur during radiotherapy (intrafractional) or between two radiotherapy sessions (interfractional), which must be taken into account during the course of treatment in order to be able to correct the location of the radiotherapy if necessary. This CD Laboratory endeavours to increase the geometric precision of the radiation application by means of surface information obtained in real time and X-ray imaging. The implementation is based on the development of software tools using artificial intelligence (AI) methods to track and correct tumour movements in real time, which will subsequently be implemented and evaluated clinically. The development of automated quality assurance processes and an improved correlation of internal and external anatomical structures with the treatment parameters are essential for evaluating the therapeutic benefit.
The adaptation of radio-oncological treatments to the individual, patient-specific tumour characteristics is the second pillar of this CD Laboratory, taking into account biological factors and, above all, tumour response. The tumour response in the course of radiotherapeutic treatment is recorded by longitudinal morphological and functional magnetic resonance imaging. Quantitative and qualitative image information from e.g. patients with ENT or gynaecological tumours is used for image analysis and evaluated with regard to the radiation dose. Adaptive therapy concepts are developed and evaluated for subsequent clinical research.
The establishment of continuous data transmission within the framework of this CD Laboratory will enable a data cycle by linking "real world" data consisting of morphological and functional image information, dosimetric data and therapy results (from the doctor's and patient's perspective). The aim is to integrate the knowledge gained from this directly into the therapy process.
In summary, this CD Laboratory enables the combination of two essential principles of current personalised radiation oncology: new technical approaches in real-time imaging and modern tumour biology-oriented adaptive treatment concepts are enhanced by automated prospective data acquisition and evaluation. This links key aspects of image-guided, adaptive radiation oncology and can be directly integrated into the clinical decision-making process and used as a basis for continuous therapy optimisation.

Christian Doppler Forschungsgesellschaft
Boltzmanngasse 20/1/3 | 1090 Wien | Tel: +43 1 5042205 | Fax: +43 1 5042205-20 | office@cdg.ac.at


